How Poor Gut Motility Plays a Role in GERD, IBS, SIBO, Constipation & More
You’ve probably heard the term ‘motility’ thrown around a lot on social media when it comes to discussions around IBS, SIBO and gut-health.
Further - you’ve probably heard that bloating, gas, irregular bowels (constipation/diarrhea), early fullness with meals, nausea, and reflux are all symptoms of ‘dysmotility’.
And so you’ve come to the conclusion - YES! These are symptoms I am experiencing a lot. I must have an issue with motility.
Well, motility is a complex topic and ‘dysmotility’ (aka abnormal motility) can present in different ways and conditions.
Let’s get into what dysmotility is, common symptoms depending on location, causes of dysmotility, and how we can improve our gut motility for improved digestion!
What is Dysmotility?
Dysmotility refers to a series of related conditions in which the muscles of the gastrointestinal (digestive) tract or the nerves that control them do not work as they should.
This means that 1) the rate at which food passes through the digestive system, and 2) the rate at which waste is excreted is abnormally slow or irregular.
Bowel dysmotility can lead to very unpleasant symptoms including diarrhea, constipation, bloating, cramping and abdominal pain.
The symptoms that appear depend on which part of the digestive tract is affected. Various parts of the bowel can be affected, and this will impact your symptoms.
Symptoms of Dysmotility
If you have dysmotility in the upper digestive tract (esophagus and stomach), you may experience:
Loss of appetite
Weight loss
Heartburn
Upper abdominal pain or discomfort
Nausea
Vomiting
Feeling full very quickly when eating
If you have dysmotility in the small intestine, you may experience:
Abdominal pain and discomfort
Cramping
Bloating and distension
Problems with bowel movements – constipation and/or diarrhea
If you have dysmotility in the lower digestive tract (colon and rectum), you may experience:
Constipation
Lower abdominal pain and discomfort
Cramping
Bloating
Common Motility Disorders
These are common motility disorders:
Gastroesophageal Reflux Disease (GERD): Frequent symptoms of heartburn and acid regurgitation. Read more about GERD and reflux management in my post here.
Intestinal pseudo-obstruction: Abnormal motility patterns in the small intestine can lead to symptoms of intestinal obstruction (bloating, nausea, vomiting)
Small bowel bacterial overgrowth: A high concentration of bacteria in the upper part of the small intestine can lead to symptoms of bloating, pain, and diarrhea. Normally, we want low concentrations of bacteria in our small bowel. For more about SIBO & IBS, I have an article for that here.
Constipation: Infrequent bowel movements [usually less than 3 per week], passage of hard stools, and sometimes difficulty in passing stools.
Pelvic floor dyssynergia: Imbalance in the anal sphincter (too tight or strained) to allow bowel movements to occur
Diarrhea: frequent, loose or watery stools, and a feeling of urgency.
Fecal incontinence: Involuntary passage of stool.
Hirschsprung’s disease: A congenital (birth) defect that prevents the internal anal sphincter to open and allow bowel movements to occur.
Gastroparesis: Gastroparesis is a disorder in which certain symptoms occur and the stomach takes too long to empty its contents.
Achalasia: An esophageal motility disorder. It is diagnosed when there is a complete lack of peristalsis within the body of the esophagus.
How to Test for Dysmotility
Dysmotility can be hard to pinpoint through tests alone, and likely requires a combination of symptom report and medical tests from your Medical Doctor to develop an adequate diagnosis if you are experiencing gut dysmotility.
Here are some common tests that mat be used to diagnose dysmotility:
Blood tests - to diagnose medical issues causing dysmotility (such as diabetes, lupus, etc); assess malnutrition, salt imbalances.
Computerized tomography (CT) and magnetic resonance imaging (MRI) scans – these can give a look inside your digestive tract, provide a visualization of what’s going on, as well as rule out any blockages/obstructions.
Motility/transit investigations - such as esophageal manometry where a thin tube is inserted into the mouth, through the esophagus, and into your stomach. This test measures the pressure and may be used for the diagnosis of GERD or achalasia.
Hydrogen-Methane Breath Test - This test can be used to diagnose Small intestinal bacterial overgrowth (SIBO). It requires you to breath out into a device for a structured period of time to measure your hydrogen and methane gas levels after consuming a lactulose or glucose solution.
Biopsy - a sample of the intestines will be extracted and tested for the above diseases.
What Can Cause Dysmotilty?
As we’ve discussed, there are quite a few conditions that involve dysmotility. There usually isn’t a clear reason for the cause, however in those with IBS and SIBO, dysmotility (imbalance in the microbiome) is generally a major underlying contributor to poor motility.
Medical conditions can be secondary risk factor to a declining function in gut motility. These key conditions include: Diabetes, Lupus, Parksinsons, and Multiple Sclerosis. These medical conditions often affect the nerves of muscle contraction therefore, impacting the muscles of digestion [1].
DYSBIOSIS & DYSMOTILITY
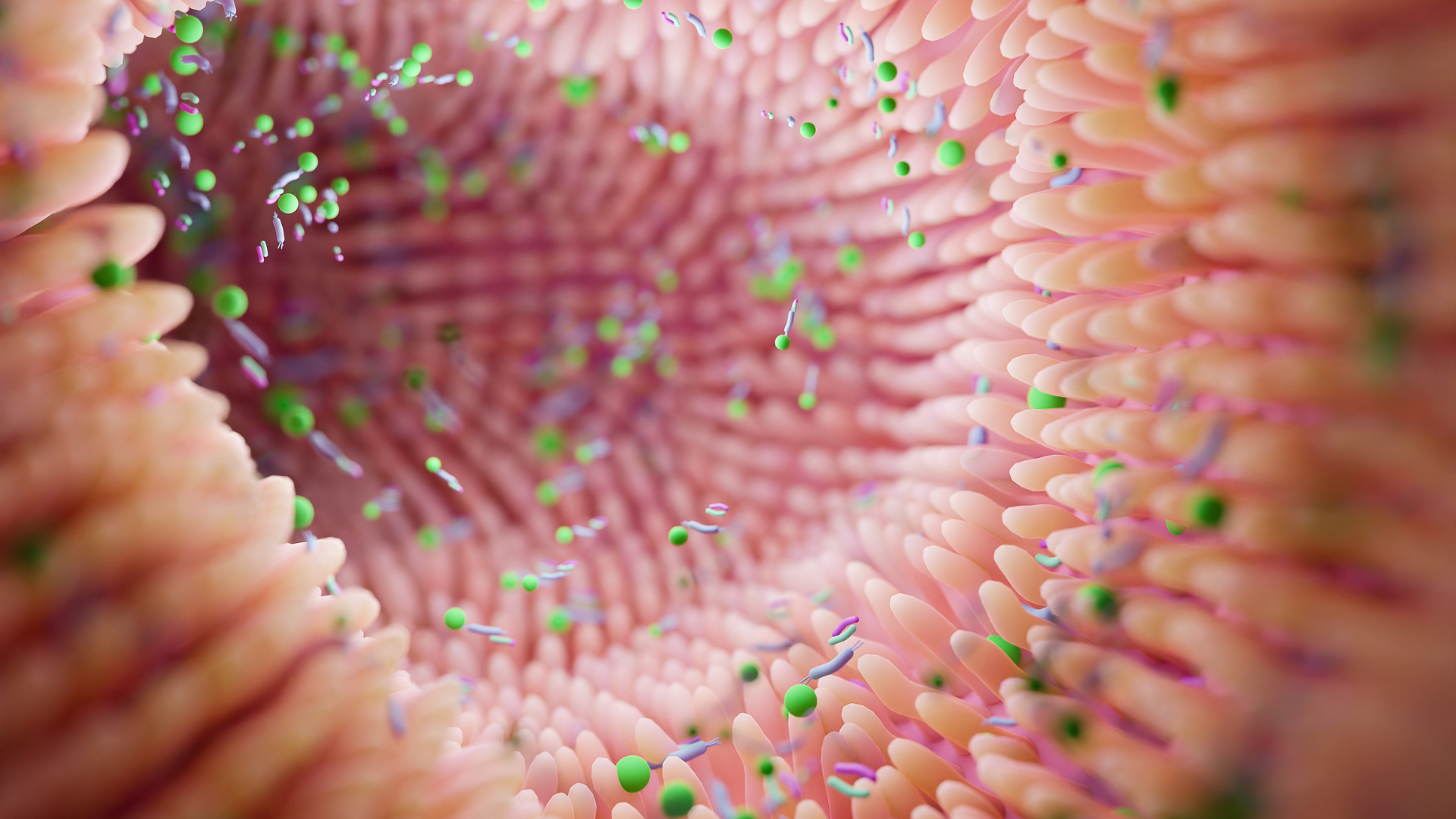
Dysbiosis refers to an imbalance of the microbial community in the gut, where the number of harmful bacteria may increase and the number of beneficial bacteria may decrease. This can lead to a variety of health problems, including issues with gut motility.
Gut motility refers to the movement of food and waste through the digestive system. When the gut microbiome is in balance, the beneficial bacteria help to maintain the health of the gut lining and promote regular contractions of the intestinal muscles, which are necessary for the proper movement of food and waste through the digestive tract.
However, when there is dysbiosis, harmful bacteria can disrupt the balance of the gut microbiome, leading to inflammation and damage to the gut lining.
This inflammation and damage can impair the regular contractions of the intestinal muscles, leading to slow gut motility or even constipation.
In addition, dysbiosis can also lead to the overgrowth of harmful bacteria, such as Clostridium difficile, which can produce toxins that further damage the gut lining and impair gut motility.
Overall, dysbiosis can cause issues with gut motility by disrupting the balance of the gut microbiome, causing inflammation and damage to the gut lining, and promoting the overgrowth of harmful bacteria.
SIBO & DYSMOTILITY
In the case of SIBO, altered gut microbes in the small bowel can contribute to the symptoms experienced such as pain, bloating, gas and distention after eating.
During periods of fasting (aka time without eating), a migrating motor complex (MMC) develops approximately every 90-120 minutes to sweep residual debris (food, bacteria) through our digestive tract. Research has demonstrated that abnormalities in the MMC function may predispose to the development of SIBO [2].
Further, SIBO may also cause disruption of the MMC as per experimental models [2]. The MMC is an important cleansing wave that helps to keep bacteria out of our small bowel. However, in the case of SIBO it’s function becomes disrupted, or is disrupted due to underlying issues, and this results in the high recurrence rates of SIBO after treatment (as bacteria continue to get pushed back into the small intestine.
IBS & DYSMOTILITY
In the case of Irritable Bowel Syndrome, where one experiences bloating, irregular bowel movements, and pain, the motility may be exacerbated by factors including poor diet, stress, lack of sleep or other medical conditions. Diets that are low in fiber and nutrients and/or higher in refined carbs and processed fats pose a greater risk of worsening motility [1].
Want an IBS-friendly meal plan to start supporting your motility for better symptom management? Grab my IBS Support (Low-FODMAP) meal plans here!
Treatments for Dysmotility
The type of treatment will depend on the cause of the dysmotility.
Many causes cannot be ‘cured’, so our focus is on addressing the underlying cause of dysmotility and also symptom management.
This can include dietary/nutrition changes, medications or supplements to modulate motility, or manipulation of the microbes in the gut-microbiome.
Diet & Lifestyle to Improve Intestinal Motility
For this post, since I am focused mainly on IBS, SIBO and functional bloating in my practice, let’s discuss some ways we can improve intestinal motility through diet and lifestyle modifications.
As mentioned, rebalancing the gut microbiome will be the most important factor to improve motility in the large and small intestine/bowel.
Fiber: Minimum of 25-35g fiber per day (higher end for males) is essential for gut motility. Foods like raspberries, chia, oats, lentils and flax seeds are excellent sources. For an IBS-friendly meal plan to meet your fibre needs, grab my low-FODMAP meal plan here!
Movement: Low-Moderate intensity movement (walking, jogging, weight lifting, yoga) can support motility.
Ginger: Ginger can help improve gut movement. Herbal teas with ginger or adding ginger to water can help support motility [3].
Potassium: Consuming enough potassium in your diet every day is essential for gut motility. Most North Americans do not get enough potassium in their diet! The big players are leafy greens, potatoes, tomatoes, edamame, and avocado.
Vagus Nerve: Strengthen vagus nerve support such as meditation, yoga, breathing, walking, sleep hygiene. Discover more about the vagus nerve in this article.
Closing Thoughts
As you can see, proper motility plays an essential role in your digestive functions and the symptoms you may be experiencing. Getting a deeper understanding of what is going on (through keeping a symptom journal, and speaking with your doctor for testing and investigation) is the first step.
From there, focusing on making changes in our diet and lifestyle to improve motility and functioning, can help you to overcome your symptoms. In my 1:1 coaching program, I help clients improve and address underlying issues such as motility with sustainable strategies, in order to manage their gut motility and find freedom from IBS & SIBO for the long term.
If you’re ready for 1:1 personalized coaching, apply for my 1-1 Gut Harmony Method Program here.

BE SURE TO FOLLOW ME HERE
References:
[1] Whitehead, W. E., & Hill, C. (2001). Gastrointestinal Motility Disorders of the 162 Small Intestine, Large Intestine, Rectum, and Pelvic Floor.
[2] Dukowicz, A. C., Lacy, B. E., & Levine, G. M. (2007). Small Intestinal Bacterial Overgrowth. Gastroenterology & Hepatology, 3(2), 112–122. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3099351/
[3] Srinivasan, K. (2017). Ginger rhizomes (Zingiber officinale): A spice with multiple health beneficial potentials. PharmaNutrition, 5(1), 18–28. https://doi.org/10.1016/j.phanu.2017.01.001