The Powerful Effect of Stress on Your Gut Health and IBS Symptoms
If you’ve been following along on my blog or social media, you’ve probably noticed that I discuss the gut-brain connection, a lot.
This topic is super important, and fairly complex. I see the connection play out very often in my clients with digestive issues like IBS, SIBO and IBD. More often than not, they know that stress is a huge trigger for flare-ups. And when they come to me, many are often in a high-stress state due to their life commitments, work, family, etc.
But also more often than not, they don’t realize how much stress is actually affecting their digestion and ability to heal.
So, let’s dive into this interesting topic in today’s post!
What is Stress?
Do you know what actually happens when you are stressed? You can probably think of the symptoms you experience when something stressful happens to you, such as your boss asking you to take over a presentation with short notice, or you get stuck in a delay on your connecting flight.
You know the feeling.. Heart starts racing, you feel a sense of pressure in your chest, your mind begins to race and you feel tense. Well, this is a natural reaction going on in your body!
Stress is the response of the body and mind to demands being placed on you.
When you feel threatened, the brain signals release of hormones to prepare the body to take action ("fight or flight response").
This includes cortisol (that hormone you often hear mentioned a lot in the health and wellness world!) which activates the sympathetic nervous system, increases blood sugars & stops insulin production, and tightens blood vessels.
We also experience a surge of adrenaline, which increases our heart rate to pump blood faster. The stress response turns off our parasympathetic nervous system: which is responsible for daily processes like digestion.
Normally, our body responds to the stressor, and then functions return to normal.
However, when we are chronically stressed, this system can be over-activated and can lead to adrenal fatigue and exhaustion.
Think about how something responds when you keep pushing it past it’s normal limits - it breaks down and gives up! This is what can happen if we let our stress go unmanaged for a long period of time.
Some stress can be a good thing: it can motivate us to work towards our goals and reach our potential.
However, too much stress can impair our mental health, and have a huge impact on our gut-health.
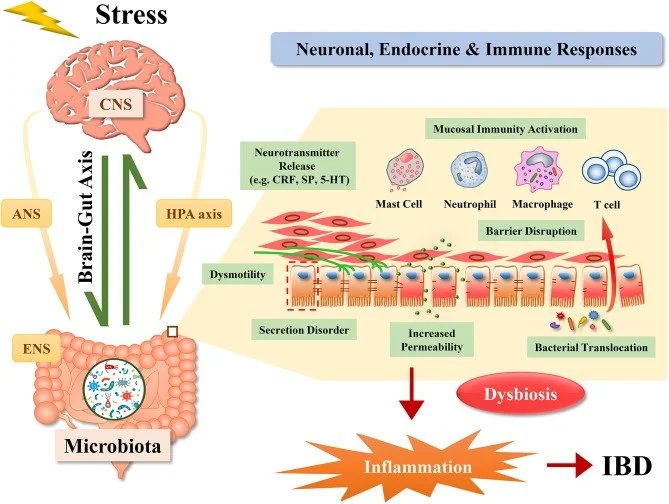
The Gut-Brain Axis
Our gut (also called our gastrointestinal tract) is the pathway from our mouth, through our esophagus, stomach, small intestine, large intestine and anus.
The gut is referred to as our “second brain”. Our gut (digestive tract) is closely connected and constantly communicating with our brain through nerve endings, neurochemicals and our gut-bacteria.
The largest nerve in the gut-brain connection is the ‘Vagus Nerve’. The vagus nerve represents the main component of the parasympathetic nervous system, which oversees a vast array of crucial bodily functions, including control of mood, immune response, digestion, and heart rate (1).
Our gut-brain axis is based on a very complex system, including the vagus nerve but also hormonal and immune links, and the influence of our gut microbiota in order to regulate our gastrointestinal homeostasis and connect emotional and cognitive areas of the brain with gut functions (2).
Pretty cool, huh?
How Does Stress Impact Our Gut-Health?
Let’s get into this topic, looking at 4 main areas that are impacted when our body is under stress, whether short or long term.
1. MOTILITY CHANGES
As mentioned, the stress response triggers the hormones cortisol and adrenaline.
Cortisol turns off the parasympathetic nervous system which is responsible for digestive regulatiion.
This is through Corticotrophin-releasing factor (CRF) which is considered to be a pivotal component in the HPA axis. It is produced by central and peripheral tissues in response to stress (3).
When CRF is released, it acts on enteric peristalsis (movement of our digestive tract) which is thought to play an important role in functional and organic disorders, such as IBS and IBD (3).
When there are changes in how peristalsis is occurring, this can result in changes in our motility. This can result in the early fullness, increase in bloating and distention, as well as changes in colonic movement (aka diarrhea/loose stools or constipation) that is experienced with stress.
2. CHANGES IN EATING PATTERNS
How does stress impact your eating choices? Take a moment and think about it.
For many, psychological stress can alter our eating choices. Some people tend to lose their appetite, and decrease the amount of food they eat. This may result in eating less nutritious foods that include fibre and nutrients that support our gut heath.
For others, stress promotes their consumption of highly palatable foods (sugary, fatty, salty). These types of foods can also depict which types of bacteria thrive, and tend to support pathogenic bacteria.
3. GUT MICROBIOME
The heightened inflammation that is triggered by stress can trigger blooms of pathogenic bacteria that encourage dysbiosis and a leaky gut (5). The principal pathogens in this group are Salmonella, Shigella, Campylobacter, invasive E coli, and Yersinia (6).
This inflammation is related to the release of catecholamines (ie. adrenaline, noradrenaline - which are released by adrenal glands when your brain senses stressor or threat (7).
Dysbiosis is when there is an imbalance of healthy and pathogenic bacteria in our gut microbiome. Ideally we want a diverse and healthy microbiome, with a higher concentration of good gut bacteria to prevent disease, support our immune system and regulate digestive function. So in both short and long term, stress can impact our gut microbiome negatively.
4. INFLAMMATION
Stress can result in increased inflammation in a few ways.
Cortisol Dysfunction:
Cortisol is a hormone that is released when we are stressed. It also naturally ebbs and flows throughout our day, and it peaks in the morning to help us with waking up and alternfulness. However, when long term stress goes unmanaged, our body can become less responsive to cortisol and dysfunction can occur.
Cortisol is a potent anti-inflammatory hormone, and its dysfunction can result in increased chronic inflammation (8).
Low cortisol is linked with associations among inflammatory cytokines, stress-related chronic pain, and salivary hypocortisolism.
CRF (Corticotrophin-releasing factor) & Inflammation
As mentioned before, the stress response promotes growth of pathogenic bacteria. Pathogenic bacteria can degrade the mucosal layer of our intestinal tract, which can cause leaky gut and contribute to inflammation.
In addition, CRF released by stress activation can induce mast cell activation. Mast cells contain ‘histamine’, which is an inflammatory protein. High levels of mast cells activation is linked with many diseases, as well as food intolerances (9).
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6821654/
How Can We Improve Our Response to Stress?
I like to break this down into long term management of stress and building resilience to stress, and acute/short term ways of managing stress and calming our nervous system.
LONG-TERM STRATEGIES
These are important strategies to build up your resilience (tolerance) to stress and help you to lower your stress levels on a daily basis:
Eating enough nutrients that help us manage stress and lower blood pressure: potassium, magnesium, quality carbs, omega-3 fats, Vitamin D
Sleep hygiene
Staying active
Creating boundaries and saying no to events/responsibilities that don’t serve you
Hydration
Daily mindfulness: journaling, meditation, walking, breathing exercises
SHORT-TERM STRATEGIES
When you experience an acutely stressful event, some ways to support your vagus nerve and lower your stress levels include:
Meditation
Deep breathing
Journalling
Gentle movement: walking, yoga, light cycling
Want to know more about supporting your vagus nerve? See my article here.
Final Thoughts
Our gut-brain connection is a necessary consideration when looking to support our gut health. While we can’t avoid stress entirely, managing acute stressors before it turns into chronic stress and leads to burnout is extremely important.
This is why my coaching program for IBS and gut-health involves an integrative and holistic framework. In my Gut Harmony Method Program we will go through a deep dive into your health & digestive history, and work on integrative strategies including stress management from diet and lifestyle to support your gut-brain connection.
Are you looking for 1-1 support for IBS and SIBO? Apply for a free 30-minute Clarity Call here. We will discuss your health goals & history, and then which of my services would be the best fit for your journey.
Feel free to pop any questions below, and for more tips on gut health & IBS, follow me on my social media @leighmerotto_rd

BE SURE TO FOLLOW ME HERE
References:
https://www.frontiersin.org/articles/10.3389/fpsyt.2018.00044/full#B1
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7213601/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6821654/