IBS Explained: Symptom Drivers, Root Causes and How to Find Lasting Relief
Have you been diagnosed with Irritable Bowel Syndrome (IBS)? If so, you probably left your doctor’s office with a minimal amount of information, and so you’re looking to learn more about it.
Well, you’ve come to the right place! In this article, we do a deep dive into an area I am very passionate about – IBS. We will discuss the root causes, diagnosis, and key symptoms of IBS based on current evidence. I will also get into my management and treatment philosophy for IBS as a Gut Health Dietitian who works primarily with clients with IBS. Let’s get into it!
What is Irritable Bowel Syndrome (IBS)?
IBS is a chronic, functional gut disorder characterized by abdominal pain or discomfort along with a range of other symptoms, including bloating, diarrhea, constipation, or alternating episodes of both.
THE MAIN SYMPTOMS OF IBS INCLUDE:
Abdominal pain or discomfort
Constipation - inadequate and/or infrequent bowel movements
Diarrhea - loose, frequent, unformed stool
Bloating - the sensation of an inflated balloon in the abdomen
Distension - a visible increase in abdominal girth
OTHER SYMPTOMS THAT THOSE WITH IBS MAY ALSO EXPERIENCE INCLUDE:
Flatulence - excessive farts / wind
Urgency - immediate need to defecate
Fatigue - tiredness, low energy
Nausea - feeling sick
Reflux or heartburn
Bowel incontinence - not being able to hold in poo
Passing mucus from your bottom
Did you know – IBS may affect 13-20% of the Canadian population at any time; however, only 40% seek help?
Many people characterize these symptoms as usual or accept them as something they just have to live with. But that isn’t the case! It is possible to find freedom from gut symptoms and achieve good digestive health.
Sub-Types of IBS
IBS is divided into three subcategories, which include:
IBS-D is when the digestive system contracts quickly, transiting products of digestion rapidly through the digestive tract, resulting in frequent, watery bowel movements (diarrhea).
IBS-C is when the digestive system contracts slowly, delaying transit time for products of digestion, resulting in hard, difficult to pass, infrequent stools (constipation).
IBS-M is when the transit time throughout the digestive tract fluctuates, causing patients to experience a mix of both diarrhea and constipation, often alternating between the two. These extreme stool consistencies can sometimes even occur within the same bowel movement.
What are the Impacts of IBS?
The significant impact of IBS is on the quality of life. Have you been living with this? If so, you’ll probably check a few of these off the list….
Low energy, fatigue
Stress (to find a washroom, the right foods, etc.)
Anxiety, depression
Increased doctor's visits
Body distrust
Distrust with food
Reduce productivity
Reduced exercise recovery
Should you be worried about medical risks? IBS is a distinct condition and does not transform into other medical conditions such as celiacs, or IBD (Crohn's or colitis). However, frequent diarrhea or constipation may increase the risk for hemorrhoids & fissures.
Diagnosis of IBS
IBS has no specific medical test (blood test, x-ray, scope, etc.) quite yet. It is usually diagnosed after other gastrointestinal conditions that may cause digestive symptoms are ruled out, such as Crohn's or colitis, celiac disease, parasite infection, anemia, etc.
However, a specific CRITERIA is used once more severe medical conditions are ruled out. This is known as the Rome IV Diagnostic Criteria* for IBS:
Recurrent abdominal pain, on average, at least one day per week in the last three months, associated with two or more of the following:
Related to defecation
Associated with a change in frequency of stool
Associated with a change in form (appearance) of stool
As per the Rome criteria: reliable only when there is no abnormal intestinal anatomy or abnormality in the biochemical (metabolic) process that would explain the symptoms. In other words, results from a physical examination and any tests are negative and appear normal.
Red Flags
As IBS symptoms can overlap with more severe conditions, such as Celiacs or Inflammatory Bowel Disease, it's essential to see an experienced doctor or gastroenterologist for proper testing and diagnoses.
If you have any of these red flags, make sure to tell your doctor so they can rule out other conditions:
Blood in stool
Anemia (low iron)
Unintentional weight loss
Fever
Symptoms that are severe or getting progressively worse
Daily diarrhea & loose stool
Bowel movements at night
Having a family history of other bowel diseases
Unreliable Tests For IBS
Many tests are widely available but not helpful in diagnosing IBS. These include:
IgG FOOD INTOLERANCE TESTS:
Also called food sensitivity blood tests
Lack of evidence supporting their use - not recommended for diagnosing a food allergy, food intolerance or sensitivity
Curious about food sensitivity testing? You may want to read: What the Science Says: This Dietitian's Honest Thoughts on Food Sensitivity Blood Tests
FECAL MICROBIOTA TESTING:
AKA stool testing (GI Map, Viome, etc.)
Stool testing may be used to rule out parasites, Crohn's disease under the guidance of a doctor, but tests cannot diagnose IBS, candida (fungal) or bacterial overgrowth.
What Causes IBS?
It can be a complex situation, however the pathophysiological factors leading to it developing can include:
VISCERAL HYPERSENSITIVTY
Visceral hypersensitivity is considered to be one of the keystone factors in the development of irritable bowel syndrome symptoms like abdominal pain and bloating. Visceral hypersensitivity is considered to be altered sensations in response to physiological stimuli. Essentially, visceral hypersensitivity means that your tolerance or threshold for pain in your intestinal lumen is lower, so even the normal functioning of your intestinal organs and digestion of food can feel painful.
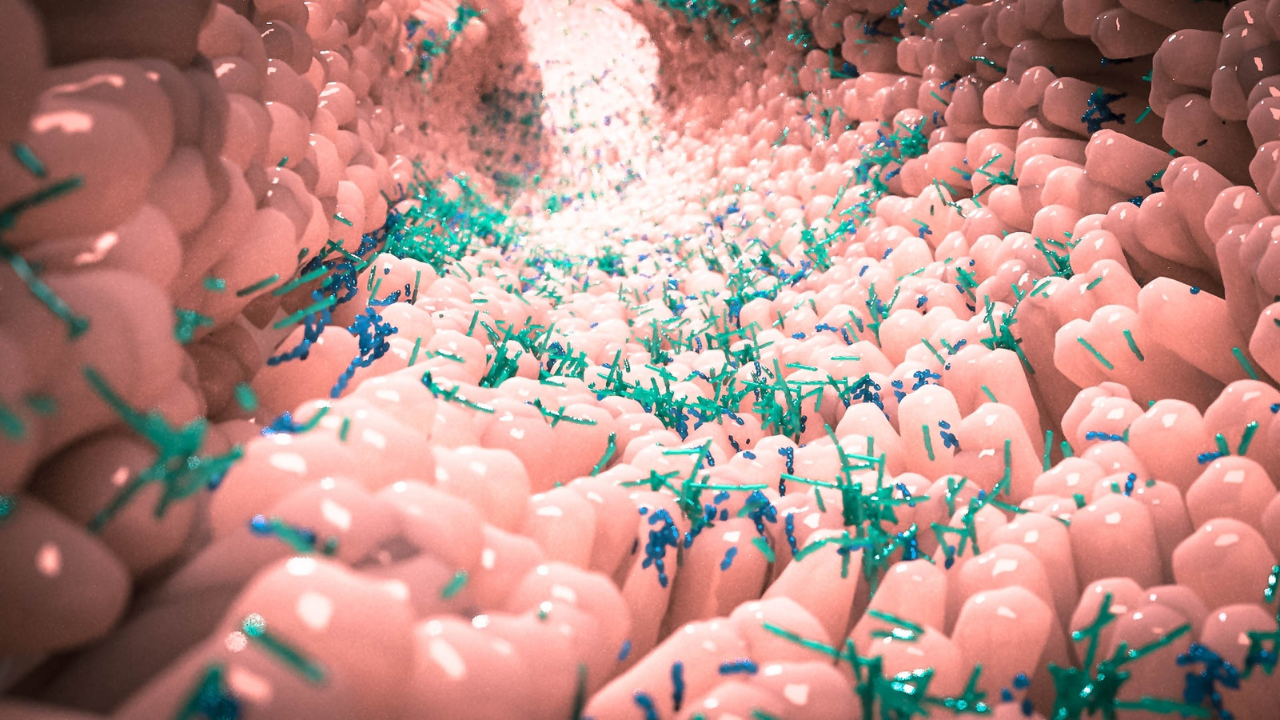
DYSBIOSIS
People with IBS quite often have an imbalance of ‘good’ and ‘bad’ microbes in their gut (fungi, bacteria, methanogens, etc). This could be due to past infections, stress, poor diet, post-pregnancy, celiac disease or other risk factors contributing to an imbalance in the gut microbiome.
SIBO & IMO
SIBO and IMO are very common types of dysbiosis present in those with IBS. SIBO (also known as Small Intestinal Bacterial Overgrowth) is incredibly common in IBS, and thought to be present in around 50-60% of IBS-D cases. In addition, it is now split into a second diagnosis, IMO (Intestinal Methanogen Overgrowth) which is thought to be responsible for a large portion of IBS-C cases.
These conditions are diagnosed by a combination of symptoms, bloodwork and a positive Hydrogen-Methane Breath test.
You may want to read: IBS & SIBO - What’s the Link Between These 2 Conditions?
LEAKY GUT & INFLAMMATION
People with IBS may have an inflamed or ‘leaky’ gut that is not readily detected on routine testing but can lead to digestive symptoms such as bloating, gas, pain, nausea, as well as poor nutrient absorption and inflammation. This could be due to pollution, excess stress, medication usage, alcohol, poor diet, and a lack of good fibre and probiotics in the diet to support beneficial gut microbes.
INFECTION (FOOD POISONING AND/OR PARASITE)
Commonly, IBS can develop after a severe gut infection from a parasite or bacterial infection. This can often lead to SIBO developing, and so there is often resulting inflammation and dysbiosis. There is now a validated test for the anti-bodies that can develop after food poisoning, known as anti-CdtB and anti-vinculin. Though there isn’t a direct treatment for these anti-bodies (yet!) , it can help to better understand why IBS developed in the first place and how we can better support your treatment plan.
If you’re interested in checking out the test, there is more information here: https://www.ibssmart.com You will need a doctor’s prescription to order and interpret the results for you.
GUT-BRAIN DYSFUNCTION
The gut-brain axis plays a distinct role in IBS symptoms, and those with IBS may have dysfunction in the gut-brain connection which can be driven by excess stress, and/or mental health conditions such as anxiety, depression. This can result in changes in gut motility, gastric secretions, gut permeability and damage the microbiome.
ALTERED GUT MOTILITY
The contents of the gut may move unusually quickly or slowly, which is sometimes called ‘altered gut motility. It could be related to stress, medical conditions, medication use, lack of movement, etc.
How Do We Manage IBS & Restore Good Gut Health?
So how do we manage IBS? Several diet and lifestyle modifications can be made to manage IBS. In addition, knowing what potentially led to the development of IBS is also essential for treatment (this is also an integral part of my approach). That is why I always start with an in-depth assessment in my practice to inform our plan better.
While medications have their time & place, I believe they are often quickly prescribed for IBS, and other factors are not even discussed with patients.
DIET STRATEGIES FOR IBS
Here is an overview of the main diet strategies/ changes that I often use with my clients to support digestive health:
Avoiding high fat/greasy meals, fried foods
Meal spacing (reducing large portions, having more spaced out regular meals)
Proper hydration
Limiting gut irritants: caffeine, added sugars, fried foods, & alcohol
Avoiding spicy foods
A gluten-free diet (if non-celiac, gluten intolerance suspected)
Low-fodmap diet and/or limiting or reducing FODMAPs
Optimal fibre intake – from food and/or supplements
Time-restricted eating (i.e. 12-hour window each day)
Mindful eating
Curious about the low FODMAP Diet for IBS? You may want to read: The Importance of Working with a Specialized Dietitian Before Starting a Low FODMAP Diet
LIFESTYLE STRATEGIES FOR IBS
Exercise: regular, low-moderate movements such as walking, jogging, weight lifting or yoga
Gut directed hypnotherapy
Cognitive behaviour therapy
Stress management & supporting vagal nerve tone: mindfulness, meditation, yoga, breathing exercises
Pelvic floor physiotherapy
SUPPLEMENTS FOR IBS
I always recommend focusing on food & lifestyle first, as these are likely to bring you the most holistic benefit (i.e. also support metabolic health, hormones, mood) as well as the most cost-effective. However, some supplements can be used to optimize an IBS treatment plan. These are some I commonly use in my practice:
Peppermint oil
Probiotics
Fibre supplements
Pre-biotics
Magnesium
Prokinetics (ginger root or herbals)
Digestive enzymes
Glutamine
My tip: Work on diet & lifestyle first, then supplement to optimize if needed. Avoid taking supplements if you aren't sure (i.e. something a friend told you worked for them) - they can make things worse!
MEDICATIONS
Prescription medications for IBS could include antispasmodics, antidepressants, prosecretory agents, anti-diarrheal agents, antibiotics, serotonin agents. These have their time & place and should be used only if the above treatments are insufficient and/or not realistic for a client’s lifestyle.
How to Find Lasting Freedom From IBS Symptoms
While it may sound like there is a lot to incorporate, the priority is to dig deeper on how your IBS may have developed to find lasting freedom. From there, we would want to address any underlying issues, and then build on sustainable nutrition & lifestyle strategies to reduce inflammation, build up your gut microbiome and support your digestive health for the long term.
For most, a sustainable treatment plan will require a combination of food & lifestyle adjustments to find the right blend for you.
In my Gut Harmony Method Program we will go through a deep dive into your health & digestive history. Determine what might be contributing to your symptoms and develop a plan to help you find symptom relief and repair your gut health for the long term.
Interested in working together 1-1 to find FREEDOM from IBS for good? Apply for a free 30-minute Clarity Call here. We will discuss your health goals & history, and how to get lasting success on your gut healing journey!
Conclusion
Despite what you may have heard, IBS is a true medical condition and has some key underlying symptom drivers including altered motility, dysbiosis, enhanced gut-brain connection, and low-grade inflammation. While you may not always be able to pinpoint the exact cause, there are many strategies to find lasting relief and heal your gut for the long term.
Have questions or want to share your IBS journey? Comment below and let’s get the conversation going!
For more IBS & gut health tips, be sure to follow along with me on social @leighmerotto_rd.

BE SURE TO FOLLOW ME HERE
References:
1. Canadian Society of Intestinal Research. (2021, April 6). April is IBS awareness month. Gastrointestinal Society. https://badgut.org/information-centre/a-z-digestive-topics/ibs-awareness/
2. Chong, P. P., Chin, V. K., Looi, C. Y., Wong, W. F., Madhavan, P., & Yong, V. C. (2019). The microbiome and irritable bowel syndrome – A review on the pathophysiology, current research and future therapy. Frontiers in Microbiology. https://www.frontiersin.org/articles/10.3389/fmicb.2019.01136/full
3. International Foundation for Gastrointestinal Disorders. (n.d.). What is IBS. https://aboutibs.org/what-is-ibs/
4. National Health Service. (2021). Irritable bowel syndrome. https://www.nhs.uk/conditions/irritable-bowel-syndrome-ibs/symptoms/
5. Pimentel, M., Morales, W., Rezaie, A., Marsh, E., Lembo, A., Mirocha, J., Leffler, D. A., Marsh, Z., Weitsman, S., Chua, K. S., Barlow, G. M., Bortey, E., Forbes, W., Yu, A., & Chang, C. (2015). Development and validation of a biomarker for diarrhea-predominant irritable bowel syndrome in human subjects. PLOS ONE. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0126438
6. Pimentel, M., Saad, Long, & Rao. (2020). ACG Clinical Guideline: Small intestine bacterial overgrowth. The American Journal of Gastroenterology, 115(2), 165-178. https://pubmed.ncbi.nlm.nih.gov/32023228/
7. Pourmorady, J., Rezaie, A., Pimentel, M., et al. (2016). 1134 The utility of measuring anti-cytolethal distending toxin B and anti-vinculin antibodies in a tertiary care motility practice: A free-range experience. Gastroenterology. 150(4). https://doi.org/10.1016/S0016-5085(16)30843-5
8. Rezaie, A., Park, S. C., Morales, W., Marsh, E., Lembo, A., Kim, J. H., Weitsman, S., Chua, K. S., Barlow, G. M., & Pimentel, M. (2017). Assessment of anti-vinculin and anti-cytolethal distending toxin B antibodies in subtypes of irritable bowel syndrome. Digestive Disease and Sciences, 62(6),1480-1485. https://pubmed.ncbi.nlm.nih.gov/28451914/
9. Rome Foundation. (2016, January 16). Rome IV Criteria. https://theromefoundation.org/rome-iv/rome-iv-criteria/
10. Schmulson, M., Balbuena, R., & Corona de Law, C. (2016). Clinical experience with the use of anti-CdtB and anti-vinculin antibodies in patients with diarrhea in Mexico. Revista De Gastroenterologia De Mexcico. 81(4), 236-239. https://pubmed.ncbi.nlm.nih.gov/27681080/
11. Shah, E. D., Riddle, M. S., Chang, C., & Pimentel, M. (2012). Estimaing the contribution of acute gastroenteritis to the overal prevalence of irritable bowel syndrome. Journal of Neurogastroenterology and Motility, 18(2), 200-204. https://www.jnmjournal.org/journal/view.html?doi=10.5056/jnm.2012.18.2.200
12. Takakura, W., & Pimentel, M. (2020). Small intestinal bacterial overgrowth and irritable bowel syndrome- An update. Frontiers in Psychiatry, 11, 664. https://www.researchgate.net/publication/342837744_Small_Intestinal_Bacterial_Overgrowth_and_Irritable_Bowel_Syndrome_-_An_Update
13. Videlock, E. J., & Chang, L. (2021). Latest insights on the pathogenesis of irritable bowel syndrome. Gastroenterology Clinics of North America, 50(3), 505-522. https://www.sciencedirect.com/science/article/abs/pii/S0889855321004684?via%3Dihub
14. Wang, L., Alammar, N., Singh, R., Nanavati, J., Song, Y., Chaudhary, R., & Mullin, G. E. (2020). Gut microbial dysbiosis in the irritable bowel syndrome: A systematic review and meta-analysis of case-control studies. Journal of Academy of Nutrition and Dietetics, 120(4), 565-586. https://www.sciencedirect.com/science/article/abs/pii/S2212267219304721